You will be near death before your blood oxygen goes below ninety. Our breathing is so efficient that the blood is 90–100% oxygenated even in severely suppressed wellbeing. Shortness of breath occurs not because there is insufficient oxygen in you. Normal Oxygen Level in Blood For most people, an oxygen level of 95-100% is considered to be normal. When the level of oxygen is within this range, it is considered to be optimum for smooth functioning of the cells. A level that is below 95% is a cause for concern and warrants an examination or testing by a medical personnel.
- Normal Oxygen Blood Levels
- Normal Oxygen Level For Children
- Normal Oxygen Levels For Adults
- Normal Oxygen Level While Sleeping
- Normal Oxygen Saturation By Age
Why did my doctor prescribe oxygen for me?
Every body needs oxygen. In fact, every tissue and every cell in the body needs a constant supply of oxygen to work properly.
Oxygen gets into our cells and tissues via the lungs. The lungs breathe in oxygen from the air, then pass the oxygen into the bloodstream through millions of tiny air sacs called alveoli. Hemoglobin in the red blood cells then picks up the oxygen and carries it off to the body's tissues and cells.
Interstitial lung disease can cause inflammation and/or scarring (aka fibrosis) in the part of the lung tissue where oxygen passes into the bloodstream — the alveoli. This inflammation and/or scarring make it difficult for oxygen to move into the bloodstream. Therefore, the amount of oxygen in the blood drops, and the body's tissues and cells may not receive enough oxygen to keep functioning properly. Not enough oxygen in the bloodstream is called hypoxemia.
How did my doctor determine that I need supplemental oxygen?
The amount of oxygen in the bloodstream can be easily measured two ways:
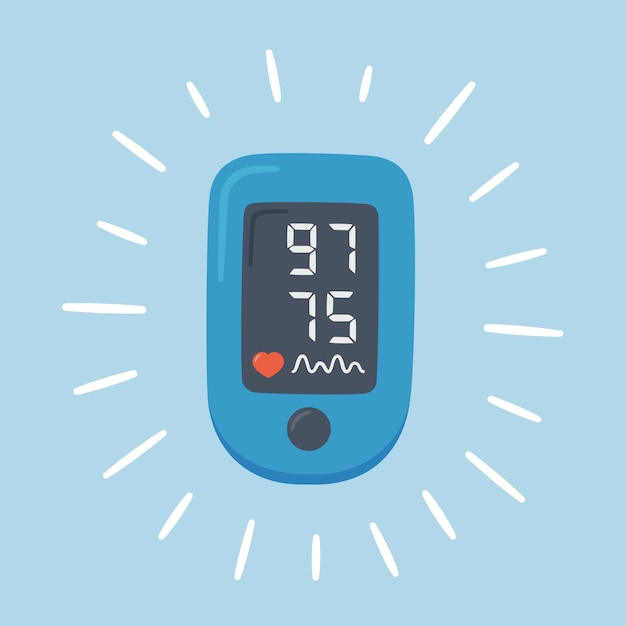
- Oximetry This is the method used most often. A small, clip-on device shines a light through your finger or earlobe and measures the amount of light absorbed by the oxygen-carrying hemoglobin in the red blood cells. By calculating the amount of light absorption, the device can measure how saturated the hemoglobin is with oxygen molecules, or O2 sat. Normally, the oxygen saturation of the blood is around 98 to 100 percent.
- Arterial blood gas study In this procedure, blood is drawn out of an artery, usually in the wrist, using a needle and syringe. The blood is then sent through an analyzer to measure the amount of oxygen gas dissolved in the blood. This result is called the arterial oxygen pressure (paO2), and is normally 80 to 100 mm Hg.
The body needs enough oxygen to keep the blood adequately saturated, so that cells and tissues get enough oxygen to function properly. Furthermore, cells and tissues can neither 'save up' nor 'catch up' on oxygen — they need a constant supply. When the oxygen saturation falls below 89 percent, or the arterial oxygen pressure falls below 60 mmHg — whether during rest, activity, sleep or at altitude — then supplemental oxygen is needed.
Your health care provider can determine your supplemental oxygen needs by testing you while you are at rest and while walking, and can also order an overnight oximetry study to test your oxygen saturation at night. A high altitude simulation test is also available to test your oxygen saturation at 8000 ft (the cabin pressure of most airliners).
When and how often do I have to wear my oxygen?
Your health care provider will write a prescription for when and how much you should wear your oxygen, based on the results of your testing. The prescription should specify the following:
- The appropriate oxygen flow rate or setting, expressed as liter flow of oxygen per minute (lpm or l/min) that will keep your saturations at or above 90 percent
- When you should wear your oxygen (for instance, during activity, overnight or continuously)
- The type of equipment that will accommodate your lifestyle needs
Why would I need to wear oxygen while sleeping?
Everyone's oxygen levels in the blood are lower during sleep, due to a mildly reduced level of breathing. Also, some alveoli drop out of use during sleep.
If your waking oxygen saturation is greater than about 94 percent on room air, it is unlikely that your saturation during sleep will fall below 88 percent. However, your doctor can order an overnight oximetry test if there is a question about your oxygen saturation levels while you are sleeping.
How do I know that I'm using the right amount of supplemental oxygen?
To determine if you're getting the right amount of supplemental oxygen, your oxygen saturation must be measured while you are using your oxygen. Your provider or a respiratory therapist from the oxygen supplier should test your oxygen saturation on oxygen while you are at rest, while walking and, if indicated, while you are asleep. As long as your saturation is in the 90s, you are getting the right amount of supplemental oxygen.
Should I buy my own finger oximeter to test my oxygen saturations?
It is probably a good idea to buy a finger oximeter, so that you are sure you are getting the right amount of supplemental oxygen. Finger oximeters are available on the internet, through medical supply companies and even in sporting goods stores.
How will using supplemental oxygen benefit me?
When a person isn't getting enough oxygen, all organs of the body can be affected, especially the brain, heart and kidneys. Wearing supplemental oxygen keeps these organs, and many others, healthy. There is evidence that, for people who are hypoxemic, supplemental oxygen improves quality of life, exercise tolerance and even survival.
Supplemental oxygen can also help relieve your symptoms. You may feel relief from shortness of breath, fatigue, dizziness and depression. You may be more alert, sleep better and be in a better mood. You may be able to do more activities such as traveling, including traveling to high altitudes.
Symptoms such as shortness of breath may be caused by something other than lack of oxygen. In these cases, supplemental oxygen may not relieve the symptom. But if tests show you are not getting enough oxygen, it is still important to wear your oxygen.
Does my need for supplemental oxygen mean that I don't have long to live?

People live for years using supplemental oxygen.
Will I always need to use supplemental oxygen?
That depends on the reason oxygen was prescribed. If your lung or heart condition improves, and your blood oxygen levels return to normal ranges without supplemental oxygen, then you don't need it anymore.
Can I become 'dependent on' or 'addicted to' oxygen?
There is no such thing as becoming 'dependent on' or 'addicted to' supplemental oxygen — everybody needs a constant supply of oxygen to live. If there is not enough oxygen in your bloodstream to supply your tissues and cells, then you need supplemental oxygen to keep your organs and tissues healthy.
Does supplemental oxygen cause side effects?
It is important to wear your oxygen as your provider ordered it. If you start to experience headaches, confusion or increased sleepiness after you start using supplemental oxygen, you might be getting too much.
Oxygen settings of 4 liters per minute or above can cause dryness and bleeding of the lining of the nose. A humidifier attached to your oxygen equipment or certain ointments can help prevent or treat the dryness. For more information, see 'Higher Oxygen Flows' in Your Oxygen Equipment.
Will I be able to go out and about with my oxygen equipment?
The goal is to have you continue as many of your usual activities as you can. You should work with your health care provider and oxygen supply company to get oxygen equipment that will allow you to do these things. Choosing the right type of equipment for you and your lifestyle is very important — the right ambulatory oxygen equipment can play a major role in improving quality of life.
Next:
Supplemental Oxygen Index:
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Related clinics
Lung Transplant Program
400 Parnassus Ave., Fifth Floor
San Francisco, CA 94143
Recommended reading
Supplemental Oxygen
Find Supplemental Oxygen Resources including, The Need for Supplemental Oxygen, Your Oxygen Equipment, Oxygen Safety, Traveling With Oxygen, and more.
FAQ: Cyclophosphamide
Cyclophosphamide is part of a class of drugs called immunosuppressants that suppress the immune response and reduces inflammation in the lungs. Learn more.
FAQ: Methotrexate
Commonly asked questions regarding Methotrexate including, recommendation, precautions, possible side effects, suggested monitoring and more.
FAQ: Mycophenolate

Commonly asked questions regarding Mycophenolate including recommendation, precautions, possible side effects, suggested monitoring and more.
FAQ: Prednisone
Commonly asked questions regarding Prednisone including, the reason for recommendation, special precautions, possible side effects, monitoring, and more.
GERD in ILD Patients
Normal Oxygen Blood Levels
Many studies have shown a link between GERD & lung disease, including interstitial lung disease (ILD). The reason for this relationship is unclear. Learn more.
ILD Nutrition Manual
Nutrition Manual for Interstitial Lung Disease including, General Guidelines for Eating Healthy, Body Mass Index, Increasing Protein in Your Diet and more.
Normal Oxygen Level For Children

ILD Resources
Normal Oxygen Levels For Adults
Patients living with interstitial lung disease (ILD) will find numerous resources listed here, offering information and support.
Pulmonary Hypertension and Interstitial Lung Disease
Pulmonary hypertension, or PH, occurs when blood pressure in the lungs becomes elevated, and can be caused by a thickening of the pulmonary artery walls.
Normal Oxygen Level While Sleeping
Pulmonary Rehabilitation for ILD Patients
Normal Oxygen Saturation By Age
Pulmonary rehabilitation is a comprehensive program for lung disease patients whose symptoms are impacting their everyday activities. Learn more here.
