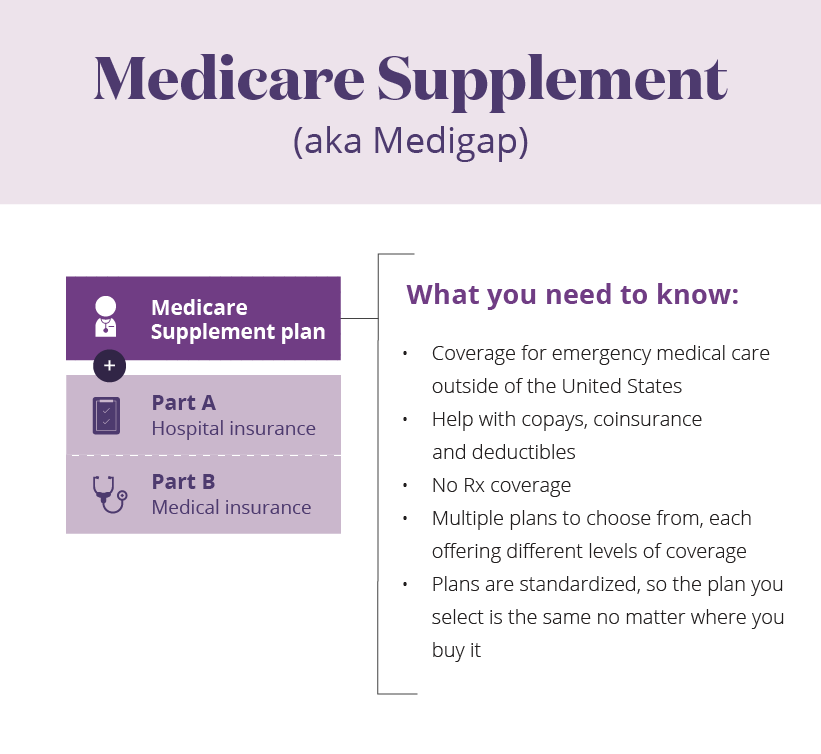
When you visit a provider or facility that takes both forms of insurance, Medicare will pay first and Medicaid may cover your Medicare cost-sharing, including coinsurances and copays. Medicaid can provide premium assistance: In many cases, if you have Medicare and Medicaid, you will automatically be enrolled in a Medicare Savings Program (MSP). Our Medicare Advantage plan, SelectHealth Advantage (HMO, HMO-SNP), offers medical and pharmacy benefits together in one simple plan.
The answer is sometimes. However, providers must be very careful to consider the implications of waiving beneficiary co-pays. Primarily, waiving co-pays may trigger The Anti-Kickback Statute.
The Anti-Kickback Statute provides in relevant part:
Whoever knowingly and willfully offers or pays any remuneration (including any kickback, bribe, or rebate) directly or indirectly…, in cash or in kind, to any person to induce such person to refer an individual [for] any item or service for which payment may be made … under a Federal health care program, … shall be guilty of a felony.42 U.S.C. § 1320a-7b(b).
Basically, the statute prohibits giving anything of value in order to induce referrals for business covered by Medicaid and other federally funded health care programs, and may apply to any transaction between providers and program beneficiaries.
However, the statue does not apply if a health care provider acts without any intent to induce improper referrals. In addition, the provider must know about the law, and act “with the specific intent to violate the law.” Hanlester Network v. Shalala, 51 F.3d 1390 (9th Cir. 1995).
Thus, actions taken in good faith for the benefit of patients or program beneficiaries without any improper intent to generate referrals or violate the law do not implicate Anti-Kickback.
The Department may examine any transaction that could generate improper referrals, especially those in which a provider offers free or discounted items or services to program beneficiaries, or those that would otherwise promote over-utilization or create a risk of fraudulent claims. See OIG Special Advisory Bulletin, Offering Gifts and Other Inducements to Beneficiaries (8/02).
Copays and deductibles help discourage unnecessary services and lower the cost of government programs. A provider’s routine waiver of copays and deductibles may create an incentive to over-utilize program resources and violate the Anti-Kickback Statute. See OIG Special Fraud Alert (12/94).
The OIG has set out some safe harbor guidelines. Waiving Medicaid and Medicare copays or deductibles does not violate the Anti-Kickback Statute if: Rotating forklift.
- the waiver is not offered as part of any advertisement or solicitation;
- the provider does not routinely waive coinsurance or deductibles; and
- the provider waives the coinsurance and deductibles after determining in good faith that the individual is in financial need or reasonable collection efforts have failed.
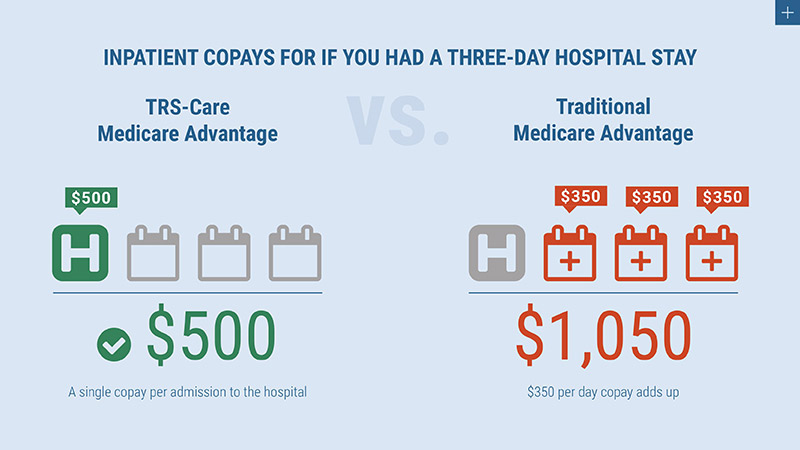
Medicare Advantage Deductibles And Copays
The beneficiary’s “financial need” will depend on the individual’s circumstances. Providers should have a written policy and guidelines in place showing consideration of factors such as the local cost of living, the patient’s income, assets and expenses, and the scope and extent of the patient’s medical bills. The documentation of financial need should be placed in that patient’s file to prove that the analysis was undertaken and the policy was followed. In addition, collection should always be attempted.
By taking these factors into consideration, a Provider may greatly reduce the risk of being flagged for fraudulent waiver of copays.
Deductibles For Medicare Advantage Plans
For more information, contact DJ Jeyaram at DJ@Jeylaw.com or 678.325.3872.
